Diabetes Care 2024;47(Supplement_1):S219–S230
https://doi.org/10.2337/dc24-S011
The American Diabetes Association (ADA) “Standards of Care in Diabetes” includes the ADA’s current clinical practice recommendations and is intended to provide the components of diabetes care, general treatment goals and guidelines, and tools to evaluate quality of care. Members of the ADA Professional Practice Committee, an interprofessional expert committee, are responsible for updating the Standards of Care annually, or more frequently as warranted. For a detailed description of ADA standards, statements, and reports, as well as the evidence-grading system for ADA’s clinical practice recommendations and a full list of Professional Practice Committee members, please refer to Introduction and Methodology. Readers who wish to comment on the Standards of Care are invited to do so at professional.diabetes.org/SOC.
Chronic Kidney Disease
Screening
Recommendations
- 11.1a At least annually, urinary albumin (e.g., spot urinary albumin-to-creatinine ratio [UACR]) and estimated glomerular filtration rate [eGFR] should be assessed in people with type 1 diabetes with duration of ≥5 years and in all people with type 2 diabetes regardless of treatment. B
- 11.1b In people with established chronic kidney disease (CKD), urinary albumin (e.g., spot UACR) and eGFR should be monitored 1–4 times per year depending on the stage of the kidney disease
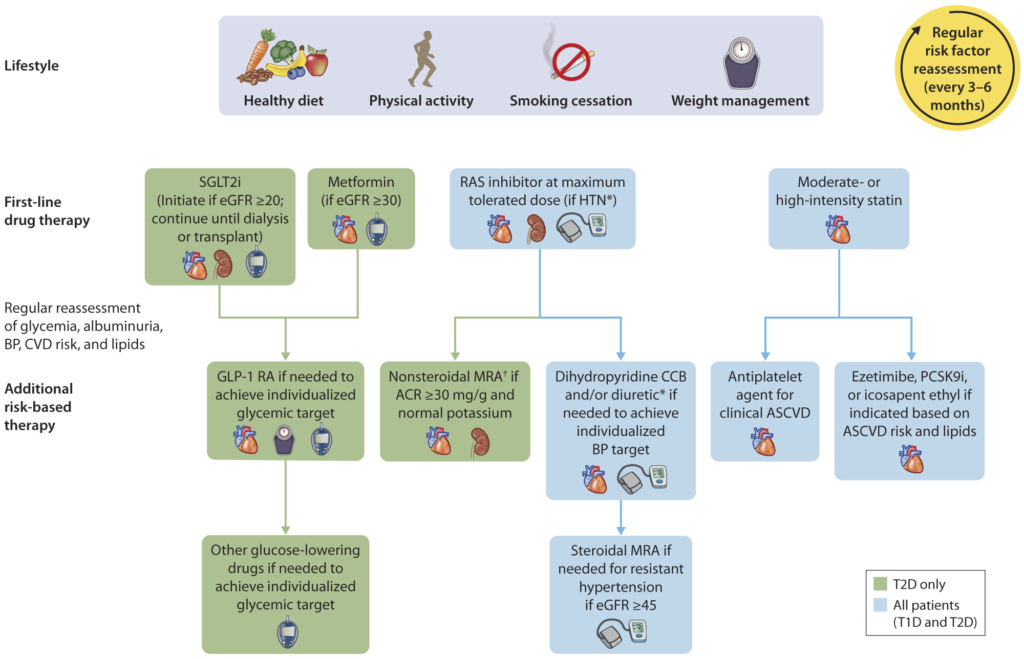
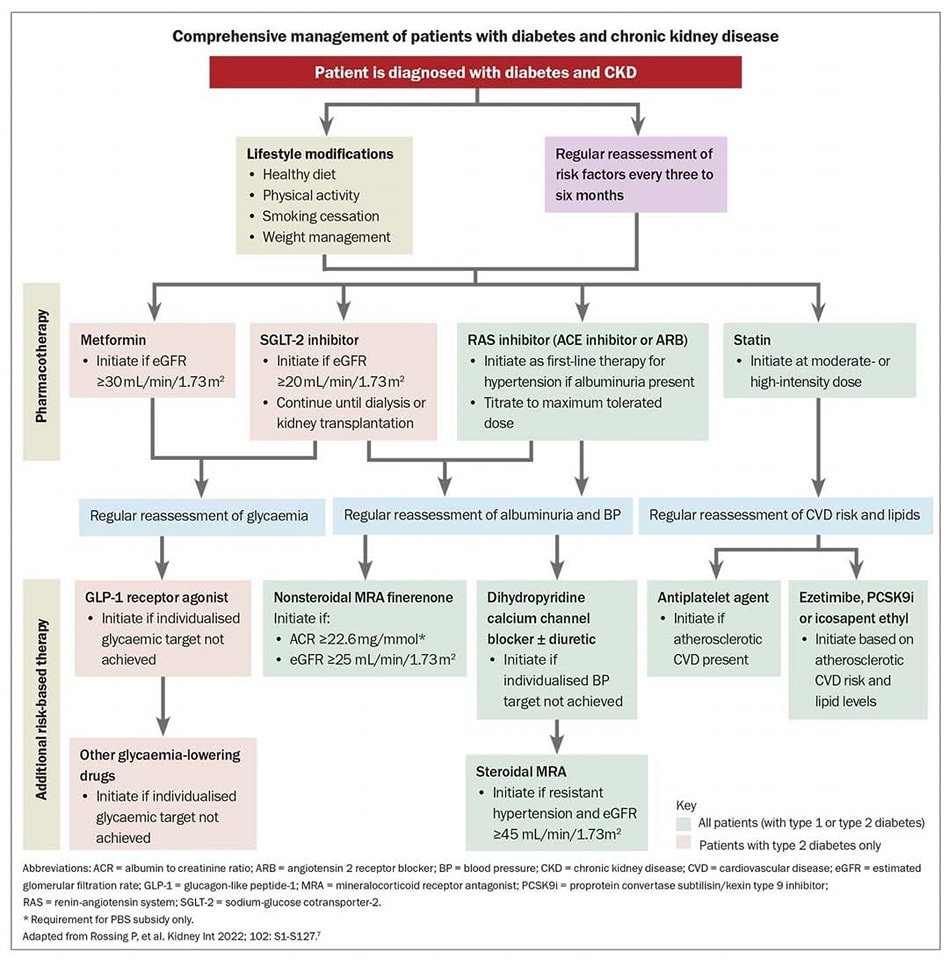
- 11.2 Optimize glucose management to reduce the risk or slow the progression of CKD. A
- 11.3 Optimize blood pressure control and reduce blood pressure variability to reduce the risk or slow the progression of CKD and reduce cardiovascular risk. A
- 11.4a In nonpregnant people with diabetes and hypertension, either an ACE inhibitor or an angiotensin receptor blocker (ARB) is recommended for those with moderately increased albuminuria (UACR 30–299 mg/g creatinine) B and is strongly recommended for those with severely increased albuminuria (UACR ≥300 mg/g creatinine) and/or eGFR <60 mL/min/1.73 m2 to prevent the progression of kidney disease and reduce cardiovascular events. A
- 11.4b Periodically monitor for increased serum creatinine and potassium levels when ACE inhibitors, ARBs, and mineralocorticoid receptor antagonists are used, or for hypokalemia when diuretics are used. B
- 11.4c An ACE inhibitor or an ARB is not recommended for the primary prevention of CKD in people with diabetes who have normal blood pressure, normal UACR (<30 mg/g creatinine), and normal eGFR. A
- 11.4d Do not discontinue renin-angiotensin system blockade for mild to moderate increases in serum creatinine (≤30%) in the absence of signs of extracellular fluid volume depletion. A
- 11.5a For people with type 2 diabetes and CKD, use of a sodium–glucose cotransporter 2 (SGLT2) inhibitor is recommended to reduce CKD progression and cardiovascular events in individuals with eGFR ≥20 mL/min/1.73 m2 and urinary albumin ≥200 mg/g creatinine. A
- 11.5b For people with type 2 diabetes and CKD, use of an SGLT2 inhibitor is recommended to reduce CKD progression and cardiovascular events in individuals with eGFR ≥20 mL/min/1.73 m2 and urinary albumin ranging from normal to 200 mg/g creatinine. B
- 11.5c For cardiovascular risk reduction in people with type 2 diabetes and CKD, consider use of an SGLT2 inhibitor (if eGFR is ≥20 mL/min/1.73 m2), a glucagon-like peptide 1 agonist, or a nonsteroidal mineralocorticoid receptor antagonist (if eGFR is ≥25 mL/min/1.73 m2). A
- 11.5d As people with CKD and albuminuria are at increased risk for cardiovascular events and CKD progression, a nonsteroidal mineralocorticoid receptor antagonist that has been shown to be effective in clinical trials is recommended to reduce cardiovascular events and CKD progression (if eGFR is ≥25 mL/min/1.73 m2). Potassium levels should be monitored. A
- 11.6 In people with CKD who have ≥300 mg/g urinary albumin, a reduction of 30% or greater in mg/g urinary albumin is recommended to slow CKD progression. C
- 11.7 For people with non–dialysis-dependent stage G3 or higher CKD, dietary protein intake should be aimed to a target level of 0.8 g/kg body weight per day. A For individuals on dialysis, 1.0–1.2 g/kg/day of dietary protein intake should be considered since protein energy wasting is a major problem in some individuals on dialysis. B
- 11.8 Individuals should be referred for evaluation by a nephrologist if they have continuously increasing urinary albumin levels and/or continuously decreasing eGFR and/or if the eGFR is <30 mL/min/1.73 m2. A
- 11.9 Promptly refer to a nephrologist for uncertainty about the etiology of kidney disease, difficult management issues, and rapidly progressing kidney disease. B