https://link.springer.com/chapter/10.1007/978-3-030-74462-5_7
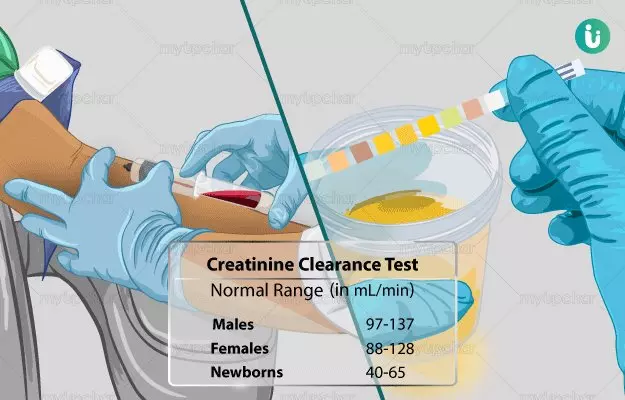
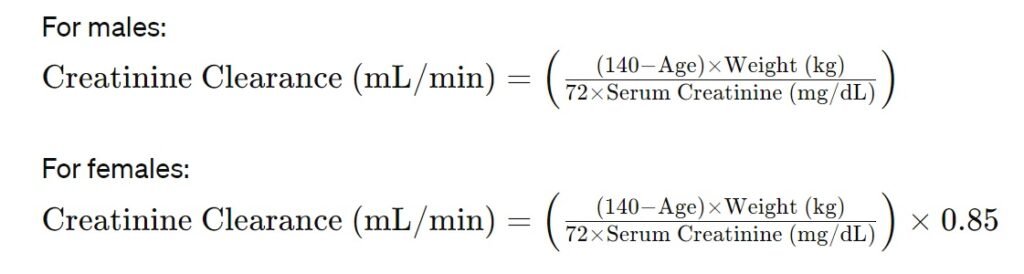
Atrial fibrillation and chronic kidney disease are on the rise worldwide and may coexist in the same patient. The rates of either thromboembolic or hemorrhagic events are increased in patients with kidney disease. Oral anticoagulation therapy, nowadays preferably with direct oral anticoagulants (DOACs), represents the cornerstone for ischemic stroke prevention in high-risk patients. However, all four available DOACs (dabigatran, apixaban, rivaroxaban, edoxaban) are eliminated by the kidneys to some extent. Reduced kidney function facilitates DOACs accumulation and therefore different dose reductions are required, with slight difference between American and European recommendations, particularly in case of severe renal impairment (creatinine clearance <30 mL/min). Overall, the use of DOACs in patients with non-end stage kidney disease and atrial fibrillation is effective similarly to warfarin, showing a better safety profile. Patients with atrial fibrillation on dialysis have been traditionally treated with warfarin, but its effectiveness for stroke prevention in this population is questionable. Some retrospective studies showed promising results with apixaban, but years will be needed for the conclusion of the ongoing randomized clinical trials. In the meantime, the management of stroke risk among patients with atrial fibrillation on dialysis will remain challenging. In patients who underwent renal transplant, DOACs may provide a potentially safer option compared to warfarin. To date, no clinical trial data is available for DOACs use in renal transplant patients, who are treated also with immunosuppressants characterized by a narrow therapeutic index. Co-administration of DOACs with immunosuppressants is a matter of concern given the risk of drug–drug interactions.






1 Comment