Popeye deformasiyası nədir?
Popeye deformasiyası, cizgi filmi qəhrəmanı Popeye-in həddindən artıq böyük bisepsinə bənzəyən şişkin biseps əzələsi ilə xarakterizə olunur. Bu vəziyyət adətən biseps əzələsini çiynə birləşdirən biseps tendonunun uzun başındakı yırtıqdan yaranır. Lakin bəzən bu hal sistem xəstəlikləri zamanıda yarana bilir. 2022 ci ildi Avropa Kardioloji Cəmiyyətinin aylıq dərgisində yayımlanmış məqalədə bir neçə Yapon və İspan alimləri bu haqda çox maraqlı araşdırma aparmışlar. Bu araşdırmaların qısa icmalı original dildə təqdim olunur.
Popeye’s sign, heart disease, and amyloidosis
Toshiya Nomura1; Fujio Fujiki2; Mitsuharu Ueda, MD, PhD1
Popeye’s sign and transthyretin amyloidosis | European Heart Journal | Oxford Academic
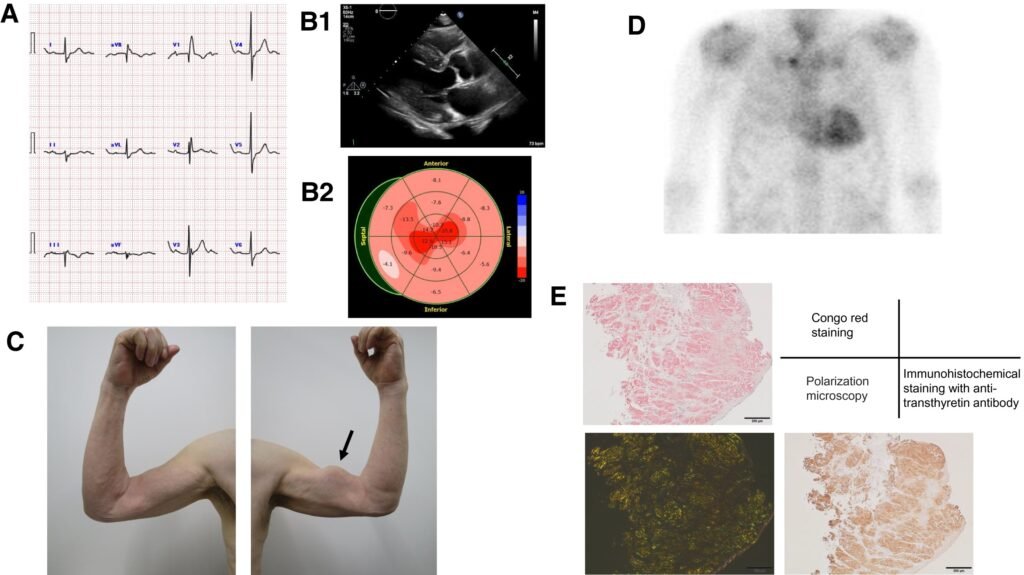
A 76-year-old man with a history of cervical open-door laminoplasty for ossification of the posterior longitudinal ligament presented to our hospital with a symptom of exertional dyspnoea. A 12-lead electrocardiogram revealed I-degree atrioventricular block (PQ interval 262 ms), left axis deviation, and complete right bundle branch block (Panel A). A transthoracic echocardiogram indicated left ventricular hypertrophy with a maximum wall thickness of 17 mm and a left ventricular ejection fraction of 61% (Panel B1). Strain echocardiogram using speckled tracking showed marked diminution of global longitudinal strain with apical sparing (Panel B2). Physical examination found subconjunctival hemorrhage in right eye, several purpuric lesions in upper extremities, and a large bulge on his left upper arm when he flexed his arm, so-called Popeye’s sign, indicating a hallmark of biceps tendon rupture (see Supplementary material online, Video S1; Panel C; arrow). A monoclonal component was not detected by serum and urine immune-electrophoresis and free light chain assays. 99mTc-labelled bone scintigraphy showed grade 3 myocardial uptake (Panel D). Eventually, endomyocardial biopsy and genetic sequencing analysis of the transthyretin gene confirmed the patient as a wild-type transthyretin amyloidosis (Panel E). Popeye’s sign is uncommon, but pivotal to diagnose transthyretin amyloidosis.
Spain Research doünload PDF content
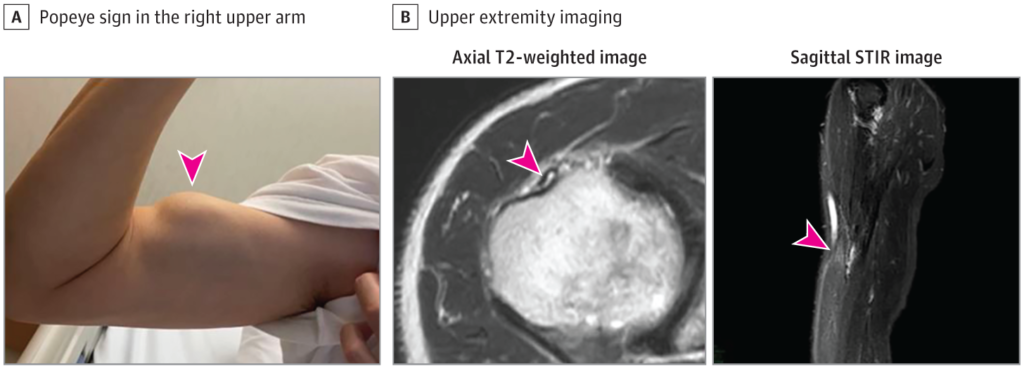
A 69-year-old man presented to our cardiology clinic troubled by breathlessness on exertion. He had a
history of hypertension, atrial fibrillation, and bilateral carpal tunnel syndrome. Physical examination
showed jugular venous distension, bilateral ankle oedema, and a bunching of the right biceps when he
flexed his arm—so called Popeye’s sign—indicating rupture of the proximal biceps tendon (figure and
video); a rupture was confirmed by an ultrasound scan. Serum N-terminal-pro-B-type natriuretic peptide
was 7088 pg/mL (normal range for patients aged 0–74 years is less than 125 pg/mL). A 12-lead
electrocardiogram showed low voltage in the limb leads, as well as a pseudo-infarct pattern in the
precordial ones (appendix). A transthoracic echocardiogram showed left ventricular hypertrophy with a
maximum wall thickness of 20 mm and a left ventricular ejection fraction (LVEF) of 40%. Cardiac MRI
showed signs of myocardial infiltration. 99mTechnetium-3,3-diphosphono-1,2-propanodicarboxylic acid
(99mTc-DPD) scintigraphy showed grade 3 myocardial uptake (figure). Serum and urine
immunoelectrophoresis and free light chain assays ruled out a monoclonal component. Genetic
sequencing analysis of the transthyretin gene found no mutations. Tying all the findings together, a
diagnosis of heart failure secondary to wild-type transthyretin amyloid (ATTRwt) cardiomyopathy was
made. The patient was treated with a combination of diuretics—namely, furosemide 80 mg twice a day,
hydrochlorothiazide 12・5 mg once a day, and spironolactone 100 mg once a day—but he did not
respond well. He remained symptomatic with advanced functional impairment and persistent signs of
systemic venous congestion.
ATTRwt, previously known as senile systemic amyloidosis, is a disease that typically affects the heart
and tendons of elderly patients. A history of bilateral carpal tunnel syndrome or, less frequently,
spontaneous tendon rupture in a patient with heart failure and preserved or mildly depressed LVEF should
raise clinical suspicion of the condition. A definitive diagnosis of ATTRwt cardiomyopathy can be
confirmed non-invasively with a positive finding on 99mTc-DPD scintigraphy, together with the absence
of a monoclonal component in serum and urine samples, and a normal genetic sequencing analysis of the
transthyretin gene. Current therapy for patients with ATTRwt cardiomyopathy is limited, with diuretics
for relief of cardiac congestion being the mainstay of treatment. However, a recent randomised, placebo
controlled trial, published in September 2018, showed a significant reduction in the risk of death and
hospitalisation from cardiovascular causes in patients with ATTRwt cardiomyopathy treated with
tafamidis, a transthyretin stabilising agent. Tafamidis is expected to be available for clinical use in the
near future.




