Aortic aneurysm and dissection
An aneurysm is a permanent, localized arterial dilation to more than 50% of the normal diameter. The histopathology of some aortic aneurysms involves medial degeneration (formerly called cystic medial necrosis), characterized by elastic fiber loss from the medial layer, loss of vascular smooth muscle cells, and proteoglycan deposition. Altered microribonucleic acid expression is implicated in increased activity of matrix metalloproteinase (MMP)-2 and -9 , which lyse elastic fibers and break down the extracellular matrix. The media within the aneurysm is also remodeled, with smooth muscle cells oriented randomly, instead of in organized layers parallel to the aortic lumen. Transforming growth factor (TGF)-β, a regulatory cytokine expressed by arterial wall vascular smooth muscle cells, modulates MMP activity. In a mouse aortic aneurysm model, disrupting TGF-β signaling prevented aneurysm formation .There are 2 TGF-β signaling pathways, and both play roles in aneurysm formation . In the canonical pathway, TGF-β binds at the cell surface to its type I or type II receptors. The complex phosphorylates Smad2 or Smad3, resulting in Smad4 recruitment and nuclear translocation, and Smad-dependent gene transcription. In the noncanonical pathway, TGF-β phosphorylates extracellular signal-regulated kinase (ERK), Jun N-terminal kinase, and p38.
Medial degeneration may (at least initially) occur as an adaptive response to wall stress in the aortic dilation zone. Per Laplace’s law, wall tension (T) equals pressure (P) multiplied by radius (R), or T = PR. Aneurysm formation increases wall tension, causing further expansion of the aneurysmal segment. As the aorta enlarges, it loses distensibility. When the tensile limit is reached, dissection may occur, but aneurysms can occur without dissection, and dissections can occur without aneurysms.
Aortic dissection
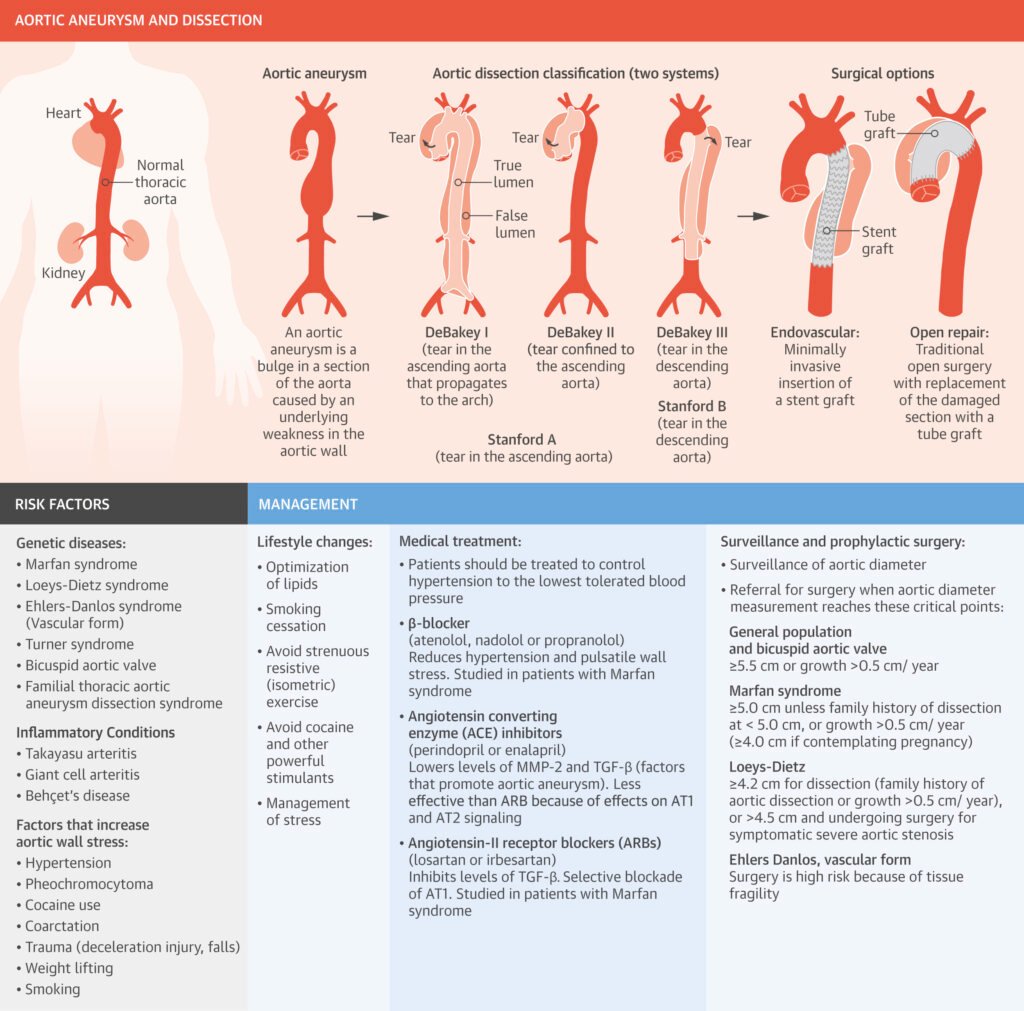
Dissection involves disruption of the medial layer, with intramural hemorrhage leading to propagation (especially when the intimal layer is also disrupted) and tracking of blood within the media. Two commonly used classification schemes are used for thoracic aortic dissection: the DeBakey scheme categorizes dissections by the site of origin; and the Stanford scheme categorizes dissections by involvement of the ascending aorta (Central Illustration). In the DeBakey classification, dissections originating in the ascending aorta are subdivided into those that propagate to the aortic arch (type I) and those confined to the ascending aorta (type II), as opposed to those that originate in the descending aorta (type III), regardless of whether they propagate distally or retrograde. The Stanford scheme is divided into type A dissections, which involve the ascending aorta, and type B dissections, which do not, regardless of point of origin .
Thoracic Aortic Aneurysm and Dissection.
Judith Z. Goldfinger, Jonathan L. Halperin, Michael L. Marin, Allan S. Stewart, Kim A. Eagle, and Valentin Fuster
JACC. 2014 Oct, 64 (16) 1725–1739